The staggering increase in opioid-related deaths in Canada cries out for novel and immediate solutions to mitigate this public health crisis. In 2022, an average of 20 lives were lost every day, twice as many as in 2019, prior to the COVID-19 pandemic.
Professors Stephanie Borgland and Tuan Trang of the University of Calgary’s Cumming School of Medicine are heeding the call through research that aims to gain insight into how opioid use disorder (OUD), a complex mental illness, changes the brain. Collaborating with people with lived experience in addiction, they will seek to accelerate the development of much-needed drug therapies by repurposing existing non-opioid medications to treat debilitating symptoms.
There are currently only four approved medications to manage OUD and the rate of relapse among individuals undergoing treatment is about 70 percent.
“I work in two different recovery centres and it’s devastating,” says Borgland, who holds the Canada Research Chair in Molecular Physiology of Addiction. “People are doing their best to stay abstinent, but they really need something to help them along, to deal with withdrawal or craving. Finding a therapeutic to support them, especially when so many are dying from this disease, is my number one goal.”
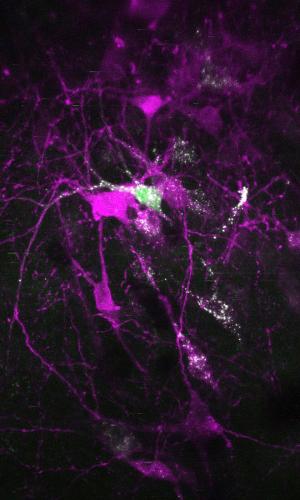
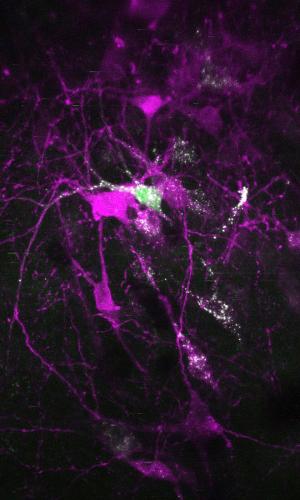
Powerful imaging technology funded recently through the CFI’s Innovation Fund will help researchers record the activity of hundreds of neurons, and of single cells within neural circuits, in rodent models. This will help them better understand how the brain’s plasticity — the ability of neural circuits to grow and change — shifts with chronic drug use. The objective is to identify targets within these neural circuits that can be blocked or enhanced with repurposed medication to help curb cravings or prevent relapse.
“Understanding the biology helps us to develop much more effective treatments at a quicker pace, and repurposing medications allows us to jump ahead further into the clinical trial stage,” says Trang, an expert in opioid pharmacology. While his team will also work on developing new drug therapies, Trang says that focusing on existing medicines for now will save on many years of testing and approvals — and could ultimately save lives.
Return to the collection called “The power to transform”