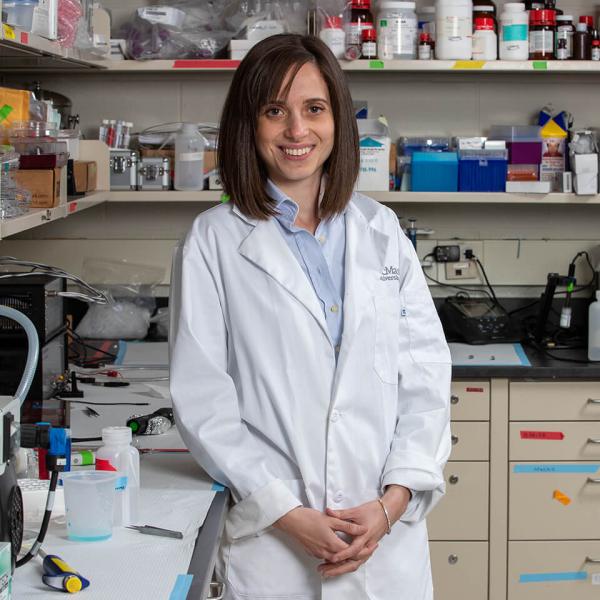
The first thing visitors notice when they step into Mousumi Majumder’s Genotoxicology Research Laboratory are the pink walls. But what really wows them is the revolutionary research that is taking place within them.
As a cancer biologist and Canada Research Chair in Genotoxicology at Manitoba’s Brandon University, Majumder and her team recently discovered a way to detect breast cancer by looking for tumour biomarkers in the blood. “That's a holy grail for cancer research, to find [a] biomarker,” she says.
Currently, mammograms are the gold standard for screening, providing an effective way to detect tumours before they are large enough to be felt. But there are drawbacks. They don’t detect all cancers. The process involves low doses of radiation, and it can be uncomfortable. And because mammograms are less effective in younger women, regular screening programs in most parts of Canada are only available to women 50 and older.
So imagine being able to get a simple blood test done instead, regardless of your age. Majumder’s breakthrough detection method opens the door to that possibility — a potential game-changer for the one-in-nine women who will be diagnosed with breast cancer in their lifetime.
Identifying telltale molecules that indicate tumours
To find appropriate biomarkers, Majumder’s team looked to microRNA (miRNA), short strands of RNA that help regulate gene expression. Of the hundreds of different miRNAs present in humans, Majumder and her team identified two specific ones — miR526b and miR655 — that were found at high levels in breast cancer tumours, as well as in the microenvironment that surrounds them.
It was an important discovery. But the real research breakthrough came when Majumder proved they could also detect measurable amounts in patients’ blood samples — and that they could detect the miRNA when tumours were still at stage one, allowing for earlier treatment and a better prognosis.
As a breast cancer survivor, Sharon Young understands how valuable this discovery could be. Today, the Brandon resident serves on the board of the Canadian Breast Cancer Network, a patient advocacy and education group, and regularly collaborates with Majumder on public awareness. “Early detection is key for survival, and having that form of screening before a tumour would develop is really exciting,” she says.
Mammograms detect around 90 percent of tumours — versus close to 80 percent using Majumder’s blood tests — but formal screening programs exclude younger women. That makes blood tests an attractive option for early breast cancer screening. Moreover, Young believes more women would choose to get screened if it involved a quick blood test rather than a mammogram. “I just think that’s an easier thing to do,” she says.
If clinical trials back up Majumder’s lab-bench results, women could be offered that option in as soon as a few years’ time.
Tracking treatment success and providing new targets
Not only could the miRNAs serve as biomarkers to detect cancer, they could also be used to assess the effectiveness of drugs. Different types of breast cancer tumours respond to different types of treatment. Regularly monitoring miRNA levels in patient blood samples could help clinicians see which drugs are working and which ones may be doing more harm than good.
But do these molecules merely indicate that cancer is present? Or do they also contribute to its growth? To answer those questions, Majumder’s team grew cancerous tumour cells in a liquid medium. Over the course of several days, the cells secreted miRNAs into the liquid.
When the researchers exposed normal cells to the liquid, the normal cells started to metastasize. That suggests the two miRNAs actually promote the spread of cancer by changing the microenvironment around a tumour — an insight that gives researchers new targets for future therapeutics.
Creating more research capacity
According to Majumder, CFI funding has been critical to her work. For starters, it helped turn an unfinished basement room at Brandon University into a 1,000-square-foot, state-of-the-art lab, which officially opened its doors in October 2023.

Meanwhile, high-throughput screening equipment and a high-performance computing workstation have dramatically increased her research capacity and produced better quality data that paved the way for publications in top-tier journals.
More space and better equipment has also allowed Majumder to double the size of her team. Today, she has 20 trainees, each one passionate about their research. “I can see clearly that they are excited,” says Majumder. “Anytime of the week, doesn’t matter what holiday it is, someone is working in the lab.”
According to Young, Majumder’s ability to humanize the research is a big reason for that excitement. “She wants to make sure that her students understand that this is about real people,” she says.
And that personal touch extends beyond the lab. Majumder regularly participates in fundraisers, gives presentations to high-school students and advocates for more research funding. “That community outreach, I think, is so important for building bridges between the lab, the university and the community,” says Young. “There needs to be more people like her.”

“Now we have all these amazing facilities and high-throughput analysis software … It is putting us on the map.”
— Mousumi Majumder, Brandon University